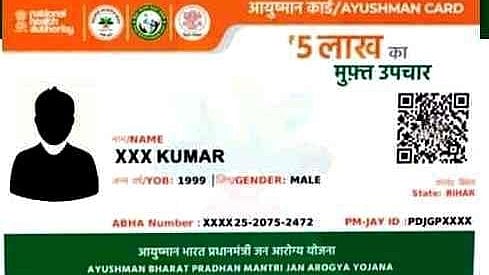
Bhubaneswar: Odisha has rolled out a unified health insurance scheme aimed at expanding access to quality healthcare for its residents. Union Health Minister JP Nadda, at an event held at Bali Jatra ground in Cuttack on Friday, inaugurated the distribution of the new Unified Ayushman Card, which integrates the Centre’s Ayushman Bharat Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) with the state-sponsored Gopabandhu Jan Arogya Yojana (GJAY).
The launch also marked the introduction of the Ayushman Vay Vandana Card, offering Rs 5 lakh in free health coverage to all citizens aged 70 and above, regardless of income or social status.
The event was attended by Union Tribal Affairs Minister Jual Oram, Chief Minister Mohan Charan Majhi, Deputy Chief Ministers KV Singh Deo and Pravati Parida, and State Health Minister Mukesh Mahaling.

Key Features of the Unified Scheme:
The initiative will benefit approximately 3.5 crore people from 1.03 crore families across Odisha. Each family will be entitled to Rs 5 lakh in annual health coverage, with an additional Rs 5 lakh specifically for women members.
Beneficiaries can avail cashless treatment at over 29,000 empanelled hospitals across the country — a dramatic expansion from the previous network of just 900 under BSKY.
Special Coverage for Senior Citizens:
Under the Ayushman Vayo-Vandana Yojana, all individuals aged 70 and above are eligible for coverage, irrespective of their socio-economic background. Families with at least one senior citizen member will receive a total health coverage of Rs 15 lakh. Eligible individuals will be issued a dedicated Ayushman Vay Vandana Card for streamlined access to services.
Financial Commitment:
To support the scheme’s implementation, the Odisha Cabinet has approved a budgetary allocation of Rs 27,019 crore over five years, ensuring sustained funding for both the central and state components of the programme