Counting data accurately and communicating it transparently is an important part of responding to COVID-19 and refining tactics as the disease evolves and spreads. This area marks not the least of the failings of the Government in the thick of fighting a pandemic that will likely leave India as one of the worst hit nations on the globe.
Take the simple case of numbers released under various heads that are not defined anywhere by the Government. Every day, the Ministry of Health and Family Welfare (MoHFW) issues numbers under three heads: active cases, cured/discharged, and deaths. We do not know how “active cases” are defined. In clinical medicine, a case is someone with significant symptoms who consults a doctor. If this is accepted as definition, then an “active case” would likely be a symptomatic person who has not fully recovered, has not succumbed to the disease and continues to be under the care of a physician. This is a person who has a) tested positive for SARS Cov-2 virus infection, b) has symptoms that require medical intervention and c) continues to suffer from COVID-19. The ‘D’ in COVID stands for disease, not merely infection detected through a positive test result. Many will get the virus, become infected but not all will develop disease. They are called infected. Those who get COVID-19 are a subset of the infected, and are, in medical parlance, known as cases.
Given this, there is the risk that India’s Infection Fatality Rate (IFR, number of deaths divided by total number of positives, i.e., those proven to be infected) is being mistaken for Case Fatality Rate (CFR, which should be number of deaths divided by total number with the disease COVID). Clearly, CFR by definition has the denominator lower than in the case of IFR, and CFR is therefore always higher than IFR.
What are these numbers in the case of India? COVID-19 cases are subsumed within the total number of infections – but dissected data of disease cases and asymptomatic infections are just not available. So, the valid denominator for CFR is unknown. There is either no transparency from officialdom, or the data collection system does not separate infections from cases of disease. We can only deduce from the data available.
Take the data for the last Saturday of June, almost three months into the lockdown. The MoHFW reported a cumulative total of 1,97,387 “active cases”, alongside 2,95,881 “cured/discharged” and 15,685 deaths (June 27 figures). The grand total comes to 5,08,953, which actually is the number of samples that tested positive and is officially described as “confirmed”. Official accounts have it that the Case Fatality Ratio (or Rate) (CFR) is 3.1% as of June 26, which is number of deaths divided by total number reported “confirmed”. But we can see that these are not strictly cases as defined in medical parlance – they are infections. Thus, 3.1 is Infection Fatality Ratio (or Rate) (IFR) rather than CFR. A reasonable view of CFR is to divide the number of deaths by those “cured/discharged” plus deaths. This is because those who were cured, discharged or died clearly had the disease and their files are closed. This way, CFR is 5.0%, which is significantly higher than 3.1% presented as CFR. We must note that in an ongoing epidemic, these are mere estimates because a) the total number infected will inevitably be larger than those tested, and b) cases of today come from infections acquired up to 14 days (incubation period) in advance.
Yet, these numbers are important because they can help us prepare for what lies ahead, judge possible changes in virus behaviour or adjust treatment protocols and plan for resources. The point is not to quibble about numbers but that honest analysis is a critical tool to fight the pandemic. Currently, the MoHFW updates data once a day, at 8 am. A reading of the releases from MoHFW and the optimistic analysis of numbers would indicate that India is putting up a good response to the pandemic. One of the datapoints released repeatedly and stressed again on the last Saturday of June is that “recoveries fast outpace the active COVID-19 cases” across the nation. According to the ministry statement of June 27: “While the number of active cases stands at 1,97,387, the number of cured cases is 2,95,880. With this encouraging status, the recovery rate is touching 58.13% amongst COVID-19 patients.” This optimism came on a day that recorded, yet again, the highest daily rise in the number of what is called “confirmed”. It was also one day before Assam, far removed from the COVID-19 hotspots so far, announced a two-week lockdown in the wake of rising number of infections in the State.
The recovery rate is presumably the percentage of those who have recovered from among the total number of “confirmed”, but the reported number is nothing to celebrate because it is widely accepted that only a small percentage have severe symptoms and most recover. In fact, all cases minus deaths are recovered – so 100 minus CFR must be the recovery rate.
So how exactly is India coping with the challenge? And how justified is the optimism, if only to ramp up morale and keep up the fight against what still remains a potent threat?
Looking at the way the virus is spreading and numbers are growing, there is no room for complacency or optimism at this stage of the pandemic. We are staring at the spectre of huge numbers of COVID-19 deaths — the wages of not investing in a proper health management system, of not planning the epidemic response well. If we take a very conservative view in which, say, only 20-30% of just the urban population (377 million, 2011 census) is infected before we can expect some level of herd immunity to kick in, even then we could lose (at the current reported IFR of 3.1%), between two and 3.5 million lives. That's a bad picture. The number may well be different, but to map that better, India will need scientifically-led randomised sample testing for antibodies (IgG titres) to reach a fair estimate of how many were infected and didn't even know about it because they were asymptomatic and fought off the infection.
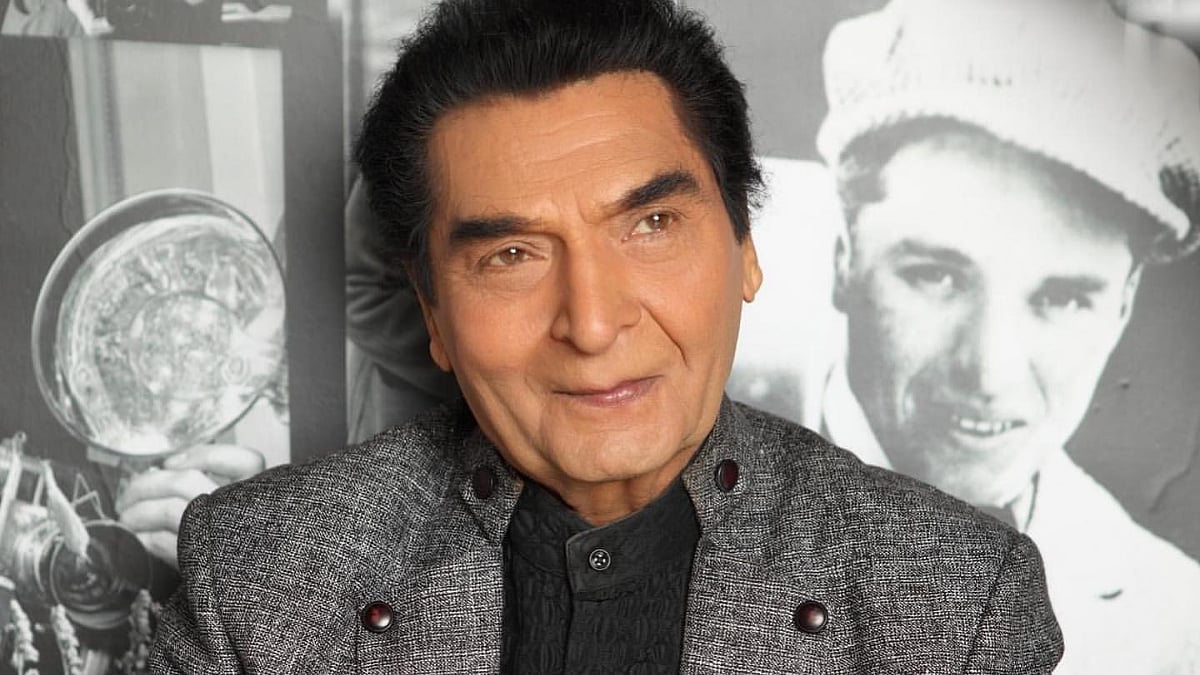
Dr T Jacob John is retired Professor of Clinical Virology, CMC Vellore, and past President of the Indian Academy of Pediatrics. Jagdish Rattanani is a journalist and faculty member at SPJIMR.
Syndicate: The Billion Press