Four in five people who have symptoms of COVID-19, get only mildly sick. For all practical purposes, that group is asymptomatic. But, if you have ongoing health issues, including liver disease, the virus is more likely to leave you seriously ill.
The link between the coronavirus and liver
While the world is euphoric that multiple COVID vaccines have now emerged to treat this new illness, one is not clear if the same saviours don’t leave those vaccinated with side effects – some of them linked to the liver. The vaccines are 95% effective, and 5% of 8 billion is still a very large number.
The American Centre for Disease Control and other experts around the world are still crunching data, but they believe the potential for harm is greater. Research on more than 10,600 people who died of COVID-19 in the U.S. found that 76% had at least one underlying medical condition. About 250 of them were noted to have long-term liver problems like cirrhosis, hepatitis, or liver disease. In some severe cases, the virus may prevent the liver from working right. One study in China showed that up to half of people with the new coronavirus, named SARS-CoV-2, had liver dysfunction at some point during their illness. It’s not clear if the reason lay with the virus or the strong medications used to fight it. Liver impairment is partly due to drug hepatotoxicity.
Currently, medicines prescribed to treat COVID-19 include oseltamivir, ritonavir/ lopinavir, ribavirin, and hydroxychloroquine sulfate, or chloroquine phosphate, which are metabolised in the liver and would produce hepatotoxicity, and the inducible liver injury can impair metabolism and excretion of the medications in turn. The postmortem biopsies of a COVID-19 patient showed mild lobular and portal activity, and moderate microvascular steatosis, which indicated that liver injury, was SARS-CoV-2 infection-related or drug-related.
Let us look at information from China. Damage in mild cases of COVID-19 is often temporary and the organ can return to normal without any special treatment. This could be due to the state of direct infection of liver cells, or due to liver cells getting caught in a war between body’s immune system and the virus with chemicals produced by our body, namely cytokines. More patients with severe disease had abnormal liver function tests than did non-severe patients with COVID-19. Those who tested positive for the virus, but did not develop symptoms, had much less involvement of the liver. In short, liver injury depends on severity of COVID-19.
Cases of acute liver failure have not been reported yet from China, or from other countries. What about people who already have liver disease? People with non-alcoholic fatty liver disease (NAFLD) or its more severe form, non-alcoholic steatohepatitis (NASH), often have cardiovascular risk factors, including metabolic syndrome, obesity and diabetes, raising the risk for severe COVID-19 complications.
Pre-existing disease
Those who have pre-existing liver disease, should they undergo check-up and LFTs to see if coronavirus has entered the liver? The answer is an emphatic NO. What has been mentioned here is abnormality of LFT in those patients who already developed COVID-19. COVID is a respiratory illness and will have symptoms pertaining to lung. Severe cases who are hospitalised alone may develop jaundice. Liver injury will not occur in the absence of respiratory illness and hence no screening tests/ LFT are indicated in patients with liver disease.
Are liver transplant recipients at higher risk for COVID-19?
Certainly. Those who have undergone liver transplant and are on immunosuppression medicines (anti-rejection medicines) are certainly at higher risk of getting this infection and logically, can end up with severe disease.
People with a weakened immune system may be unable to fight off the virus. So transplant patients have more chance of getting the virus, but paradoxically transplant recipients may not exhibit symptoms — fever, breathlessness — to begin with.
Some natural ways of keeping liver healthy
There are two major types of fatty liver disease — alcohol-induced and nonalcoholic fatty liver disease. One of the main ways to treat fatty liver disease, regardless of type, is with diet. As the name suggests, fatty liver disease means you have too much fat in your liver. In a healthy body, the liver helps to remove toxins and produces bile, the digestive protein. Fatty liver disease damages the liver and prevents it from working as well as it should.
Here are a few foods that you can include in your daily diet for a healthy liver:
1. Coffee to lower abnormal liver enzymes.
2. Greens to prevent fat buildup.
3. Vegan dairy substitutes to reduce fat buildup.
4. Fatty fish for inflammation and fat levels (vegetarians may opt for cod-liver oil).
5. Oatmeal for energy.
6. Walnuts to improve liver function.
7. Avocado to help protect the liver.
8. Milk and other low-fat dairy to protect from damage.
9. Sunflower seeds for antioxidants.
10. Olive oil for weight control.
11. Garlic to help reduce body weight.
12. Green tea for less fat absorption.
Eight thing that you should avoid if you
have fatty liver: Alcohol, added sugar, fried foods, high salt, white bread, rice, pasta, and red meat.
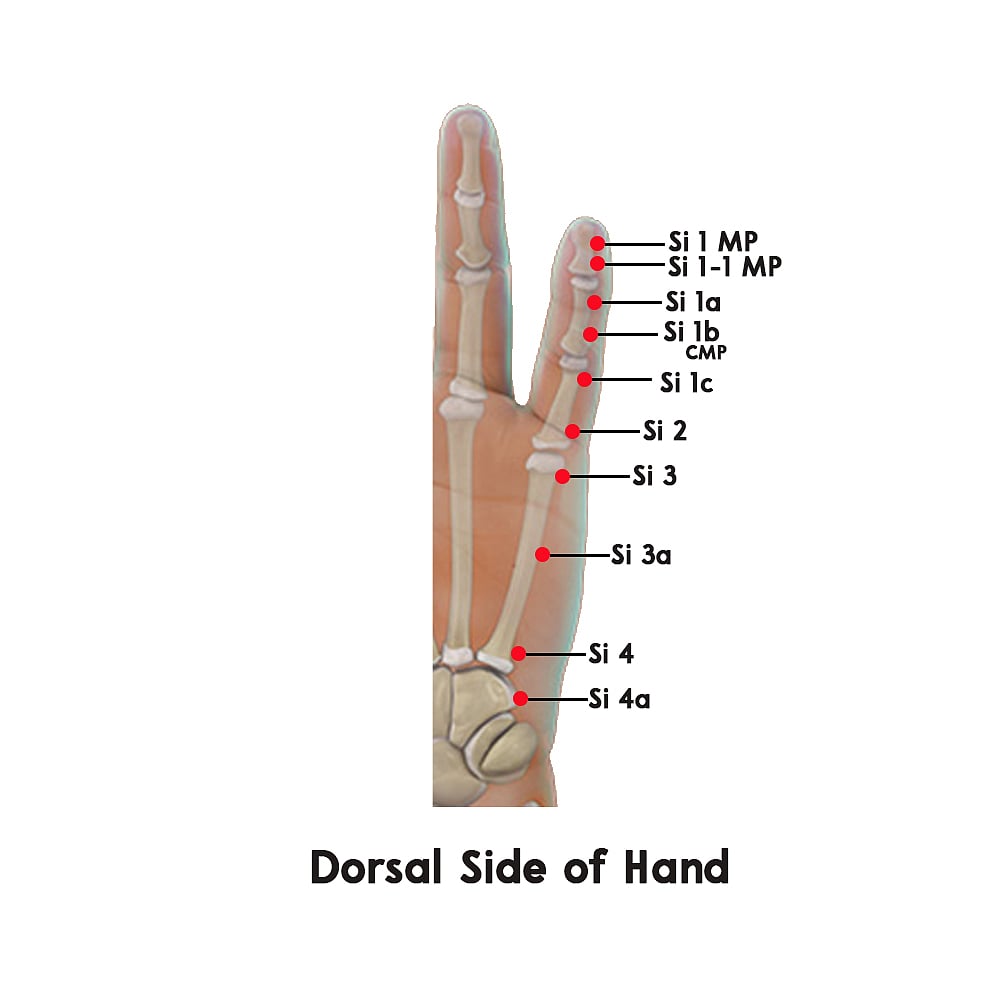
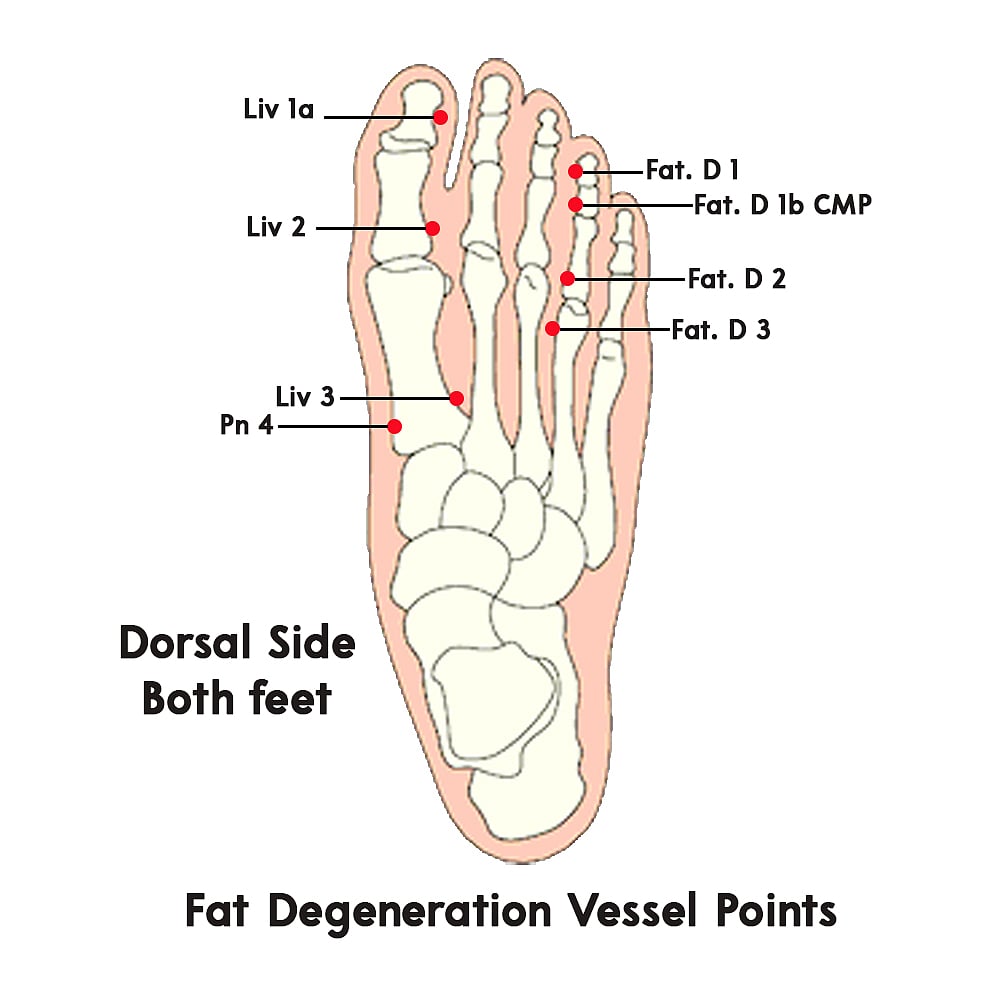
Pressure points for treatment:
By pasting methi seeds on points Fat D1, 1b Si 1a (on right food), Pn 4, Liv 1a, 2 & 3, as shown in the figure below. For treating congestion of the central veins of liver also known as Nutmeg liver, focus on these points – Liv 1, 1a, 3 & H 9.
Additional ways to treat liver disease:
Become active: Exercise, paired with diet, can help you lose extra weight and manage your liver disease. Aim to get at least 30 minutes of aerobic exercise on most days of the week.
Lower cholesterol: Watch your saturated fat and sugar intake to help keep your cholesterol and triglyceride levels under control. If diet and exercise aren’t enough to lower your cholesterol, ask your doctor about taking medication.
Control diabetes: Diabetes and fatty liver disease often occur together. Diet and exercise can help you manage both conditions. If your blood sugar is still high, your doctor can prescribe medication to lower it.
(From increasing metabolism to overcoming physical problems, Prof Luthria speaks about the art of self-healing through simple techniques. For more information on treatments and remedies, visit www.artofselfhealing.in)











